Traumatic brain injury (TBI) is a devastating clinical condition that contributes to a substantial number of deaths and cases of permanent disability. Each year over 1.5 million individuals in the United States and approximately 10 million people worldwide suffer a TBI and it has now has become one of the leading causes of morbidity and mortality in children and young adults. Typical etiologies include motor vehicle accidents and falls in adults, sports related injuries in children and young adults, and nonaccidental trauma in infants.
Traumatic Brain Injury
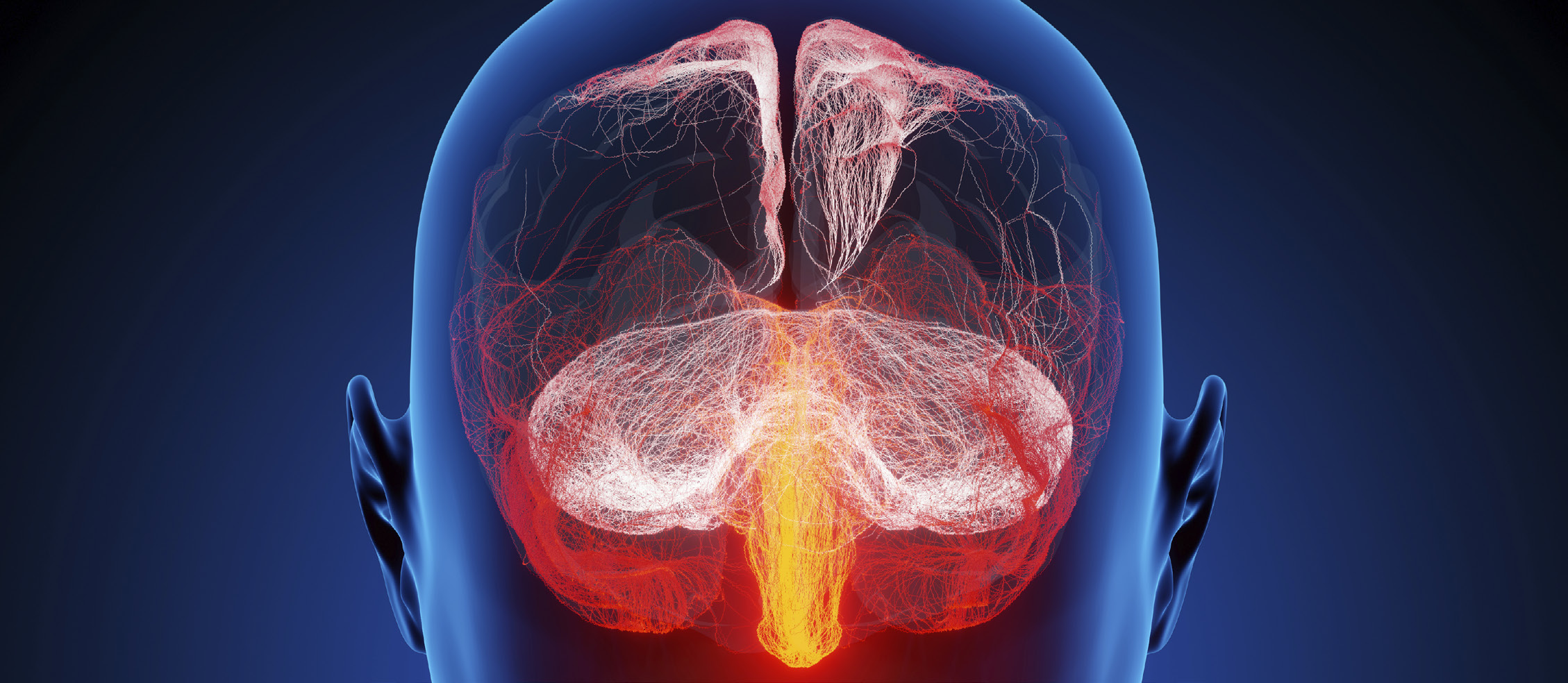
Traumatic brain injury (TBI) is a devastating clinical condition that contributes to a substantial number of deaths and cases of permanent disability. Each year over 1.5 million individuals in the United States and approximately 10 million people worldwide suffer a TBI and it has now has become one of the leading causes of morbidity and mortality in children and young adults. Typical etiologies include motor vehicle accidents and falls in adults, sports related injuries in children and young adults, and nonaccidental trauma in infants. Given the societal impact, there is a significant amount of clinical trial work being performed to evaluate traumatic brain injury. Today, there are over 400 ongoing clinical trials. As a TBI disrupts the normal function of the brain, medical imaging plays a critical role in diagnosing traumatic brain injury as well as determining the effect of treatment on the progression of intracranial pathology.
Clinical Evaluation
The clinical evaluation of patients at the time of their presentation typically uses the Glasgow Coma Scale to grade a TBI as minor, mild, moderate or severe. The chronic outcome of the patient can be described using the Glasgow Outcome Scale with the four categories being: 1. vegetative state if the patient shows no ability to obey simple commands; 2. severe disability if the patient is conscious but needs another person’s assistance for activities of daily living; 3. moderate disability for patients who are independent but disabled; and 4. Good recovery indicating the capacity to resume normal occupational and social activities. Depending on the clinical presentation of the patient, a radiologic evaluation to detect intracranial injury is performed.
Computed Tomography and Marshall Criteria
In the past, conventional plain film radiography of the skull was the primary tool used for trauma evaluation. Its role now is relegated to evaluation of penetrating traumatic injuries and to better delineate skull fractures in clinically suspected child abuse.
Today, noncontrast head computed tomography (CT) is the favored initial imaging study for suspected acute TBI given its widespread availability, speed and safety. CT has great sensitivity for detecting acute hemorrhage, hydrocephalus, for detecting herniation syndromes, fractures and evaluating for foreign bodies. It plays a critical role in determining if patients need immediate surgical treatment or can be stabilized medically. In addition to noncontrast CT, CT angiography can be performed of the head and neck to evaluate for potential vascular injury. Typical injuries in trauma include pseudo- aneurysms, dissections, vascular lacerations and carotid- cavernous fistulas. CT perfusion uses intravascular iodinated contrast to evaluate the blood flow perfusion of the brain and can be used in patients with suspected stroke as a result of TBI.
CT can also be used to categorize a subset of TBI patients at risk of developing intracranial hypertension. This classification system was proposed by Marshall et al in their landmark paper published in the Journal of Neurosurgery in 1991. Grade 1 patients had a normal CT scan and showed 9.6% mortality. Grade 2 patients had basilar cisterns present and midline shift of less than 5mm. The mortality in these patients was 13.5%. Grade 3 patients had absent or compressed cisterns with less than 5mm of shift and showed a mortality of 34%. Grade 4 patients had a shift of greater than 5mm and a mortality of 56%. These criteria are valuable in patients with severe head injury, but may be limited in less severe injuries, as well as patients with nonhemorrhagic/microhemorrhagic shear injury and posterior fossa injuries without severe edema.
Magnetic Resonance Imaging
Magnetic resonance (MRI) imaging is increasingly playing an important role in the evaluation of TBI. The typical indication involves patients with TBI whose clinical neurologic condition cannot be explained by CT. MRI provides greater sensitivity than CT for brainstem injuries, ischemia/infarct, posterior fossa injuries, and injuries that occur near brain/bone interfaces including contusions. MRI is also used in the subacute and chronic phases of TBI to provide valuable prognostic information. Key conventional MRI sequences to perform in suspected TBI patients include; fluid attenuated inversion recovery (FLAIR), gradient recalled echo (GRE) or susceptibility weighted imaging (SWI), and diffusion weighted imaging (DWI). FLAIR imaging suppresses the normal bright T2 signal from cerebrospinal fluid (CSF) and improves the conspicuity of subarachnoid hemorrhage, nonhemorrhagic diffuse axonal injury (DAI), and cortical contusions. GRE T2* weighted imaging and SWI provide increased sensitivity to the presence of blood breakdown products including deoxyhemoglobin, methemaglobin, ferritin and hemosiderin. On these sequences blood products show a sharp loss of signal intensity known as “chemical blooming artifact” and are more easily visualized, than on other MRI sequences and often CT exams.
DWI is an MR imaging sequence that is sensitive to the diffusion of water molecules within tissues. The sequence is typically used in the evaluation of suspected transient ischemic attack (TIA), and ischemia/infarct. DWI can also play a role in identifying cerebral contusions that may be missed on FLAIR and GRE imaging. In restricted diffusion, there is a reduction in apparent diffusion coefficient (ADC) that results in bright signal intensity on DWI. This is usually seen in patients with cytotoxic edema from stroke in which there is cellular swelling which limits the diffusion of water molecules in the extra- cellular space thus showing bright signal. This can also occur in neurons and axons acutely injured from trauma, where water molecules will have restricted regions to distribute, and will subsequently show increased signal intensity.
Diffusion tensor imaging (DTI) is a newer MRI technique that is related to DWI but allows for virtual reconstruction of axons and can provide images of the disrupted neurons using tractography. As opposed to DWI which primarily images the magnitude of water diffusion, DTI measures the magnitude and direction of water- associated proton diffusion. Anisotropy refers to the fact that water molecule diffusion in white matter tracts is not random and occurs in an axis parallel to the axons secondary to the microstructure of the tracts. Alterations in the microstructure, as can occur in trauma, tumor, stroke or inflammation can be imaged using this technique. Evaluation of the fiber tracts of the brain can be valuable in predicting the prognosis of patients including coma duration and potential cognitive deficits. This is especially important in patients that have incurred an acute shearing injury, known as diffuse axonal imaging (DAI). This results from rotational acceleration and deceleration forces that produce shear strain deformities in the brain. These injuries usually occur at one of three loca- tions in the brain; at the junction of the gray and white matter, in the white matter tracts of the corpus callosum, and in the dorsolateral aspect of the upper brainstem. Clinical symptoms and prognosis worsen with the depth of DAI from the surface of the brain. Using DWI and DTI, these important injuries can be detected within the first few hours after brain trauma.
Functional MR imaging (fMRI) is another research tool being evaluated for the assessment of TBI. This technique detects differences in the ratio of cerebral blood deoxy- hemoglobin to oxyhemoglobin in functioning regions of the brain while performing different tasks. As neuronal activity increases in certain portions of the brain, blood flow is increased and local blood oxygenation also increases. Ultimately in this region of brain, the amount of paramagnetic deoxyhemoglobin decreases and there is an increase in signal intensity in this region of the brain on GRE images. This exam has been typically used in patients with deficits after mild TBI to evaluate the brain’s ability to reorganize after injury.
Magnetic Resonance Spectroscopy
Magnetic resonance spectroscopy (MRS) is another tool that can be used to evaluate for traumatic brain injury. The typical brain metabolites measured with MRS include; N-acetylaspartate (NAA) a marker of axonal and neuronal functional status, creatinine (Cr) a marker for cell energy metabolism and mitochondrial function, and choline (Cho), a marker for cellular membrane integrity. Smaller concentration metabolites include gulamate, lactate and myoinositol. A reduction in NAA in acutely injured patients portends a poor recovery, while a return to normal values typically is associated with good outcomes. Increased choline peaks are typically seen in shearing injuries. Increases in Cr may be seen in repair mechanisms secondary to acute injury. It should be noted that MRS is still primarily used as a research tool and is not yet “ready for primetime” and will need more studies to fully evaluate its common use in trauma
Summary
Traumatic brain injury is a worldwide epidemic affecting greater than 10 million patients annually. The impact on the lives of patients, their families and society as a whole can be devastating. Critical information needed in the diagnosis, treatment and prognosis of these often complicated patients is derived from a combination of clinical information, including the Glasgow Coma and Outcome scores, as well as imaging findings diagnosed with CT and MRI examinations. Extensive studies in the treatment and intervention of TBI are currently being performed around the globe with primary goals of implementing prevention strategies, developing evidence- based interventions, and thus reducing the morbidity and
mortality of this devastating condition.
Volume 6, Issue 2: Traumatic Brain Injury: Medical Imaging in Clinical Trials
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.