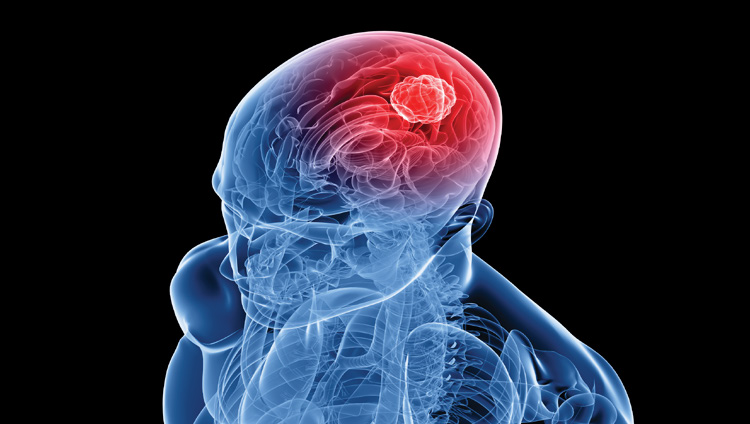
Glioblastoma multiforme (GBM) is the most common and most aggressive malignant type of primary brain tumor (gliomas). With the exception of the brainstem gliomas, glioblastoma multiforme has the worst prognosis of any central nervous system malignancy.
There are many ongoing clinical trials designed to evaluate treatment regimens for gliomas and in particular glioblastoma multiforme brain tumors; however determining reliable imaging endpoints in clinical trials remains very problematic. This is a result of the inherent growth characteristics of primary brain tumors which demonstrate extensive infiltration of the surrounding normal brain. From an imaging perspective, this often results in an imperceptible transition from normal brain to areas of gross tumor involvement.
Because gliomas usually present with an irregular shape and with infiltrative margins, the typical planar measurements used in other oncology trials are very problematic as they do not adequately assess the extent of initial, residual or recurrent disease in the brain.
To further complicate brain tumor assessments, part of the pathologic diagnostic criteria for a GBM includes the presence of necrosis. By definition then, portions of the measured tumor volumes of a GBM using existing software will include non-viable tumor. Even more problematic is the frequent presence of treatment necrosis on follow-up imaging. Dying glial cells release toxic compounds that can cause cell death in surrounding non-neoplastic tissue creating a growing mass mimicking tumor progression. Necrotic enhancing tissue needs to be separated from enhancing active tumor.
The differentiation of active tumor from treatment necrosis continues to limit the ability to assess treatment strategies for gliomas. MRI perfusion with dynamic susceptibility imaging (DSI) has become a critical tool in brain tumor follow-up in discriminating recurrent tumor and treatment necrosis. The second part of the pathologic diagnostic criteria for GBM is the presence of vascular proliferation. The basic concept of DSI involves rapid imaging while a bolus of intravenous contrast is administered. In the presence of active tumor with vascular proliferation, there will be an increase in perfusion blood volume. With treatment necrosis, there will be prominent enhancement from damaged, leaky blood vessels but there will be less perfusion blood volume caused by the loss of normal vasculature in treatment necrosis.
Despite the bleak prognosis of high grade primary brain tumors, there have been recent significant advances using the alkylating agent temozolomide (Temodar) and the anti-angiogenesis immunoglobulin bevacizumab (Avastin). However, even these treatments pose difficulty when evaluating their therapeutic effects. Avastin for example causes a dramatic response by stabilizing vessel endothelium with a prominent decrease in enhancement, edema and associated mass effect. A significant problem arose when it became apparent that Avastin causes a marked imaging and clinical response in both active tumor and in treatment necrosis. Especially problematic for imaging was the realization that Avastin normalized the abnormal perfusion blood volume for tumor preventing the identification of separate, active tumor from necrosis. Subtle, subjective T2 signal differences are all that allow the detection of progression of non-enhancing tumor in a patient on Avastin from surrounding T2 changes present in adjacent treated white matter.
To accurately evaluate brain tumors, we need software capable of providing volumetric measurements of both the non-enhancing T2 component and the post contrast enhancing component on T1 weighted images. A user defined threshold will need to be used to differentiate the signal characteristics of the tumor from the surrounding tissue and a voxel calculation will need to be made to determine the volume in cubic millimeters of the enhancing and non-enhancing tumor.
The ideal software measurement tool for brain tumor follow-up would combine the volume information of the non-enhancing T2 signal, the enhancing component and the perfusion characteristics of these separate components. Since high grade gliomas essentially always have a mixture of necrosis and residual tumor, it is critical to be able to provide separate volumes for the active tumor and the extent of treatment necrosis. Although residual active tumor may be present, determining whether the dominant process is tumor or treatment necrosis is critical to patient management and understanding the response to treatment.
As a result of the inherent growth characteristics of primary brain tumors, clinical trials designed to evaluate treatment regimens for gliomas continue to present a number of challenges. However incorporating subtle treatment effects and advanced volumetric imaging software would allow valid imaging endpoints for novel treatment agents being pursued by Sponsors.
Volume 5, Issue 8: Guidance for Sponsors: The Challenge of Quantitative Measurements of Primary Brain Tumors in Clinical Trials
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.