Recent headlines have highlighted the potential for Chimeric Antigen Receptor (CAR)-based therapies to provide clinical benefits to persons affected by lupus. Lupus is a chronic and often debilitating autoimmune disorder, and it has long posed significant challenges in treatment due to its complexities.
CAR-T Cells Target Harmful B Cells in Lupus
CAR-T cell technology, which uses genetic engineering to direct white blood cells to attack specific molecular targets, was originally proposed for treatment of HIV infection and hematological malignancies. Today there are six CAR-T products with FDA approval for the treatment of multiple myeloma and B cell malignancies, with many related and next-generation products under development. An expected and well-known side effect of these B cell-targeted therapies is “B cell aplasia”— i.e. partial or complete depletion of B cells from circulation and immune organs. In the context of anticancer treatment, B cell aplasia is considered an undesirable but manageable side effect of these therapies. Recently clinical investigators have found a way to turn what was an undesirable side effect in cancer patients into a clinical benefit for persons with certain autoimmune conditions. In these cases B cell depletion is a feature, not a bug.
T cells and B cells — both specialized white blood cells called “lymphocytes”– represent the two arms of the adaptive immune system responsible for immune memory and recall responses to vaccines and infections. Lymphocytes have an extraordinary capacity to proliferate in response to immune stimulation. This proliferative capacity allows a rapid response to an incoming threat, such as a viral infection. T cells and B cells also express specialized antigen receptors that impart specificity to the immune response, directing immune attack against foreign “non-self” targets while sparing “self” targets expressed by healthy tissue. When properly regulated these cellular features—proliferative capacity and receptor-directed specificity—largely account for the effectiveness of our adaptive immune system in protecting us from infectious disease. When dysregulated, these same features can have very serious and even deadly consequences. Lymphocytes undergoing uncontrolled proliferation can transform into lymphomas and related hematological malignancies. Lymphocytes that fail to distinguish self from non-self can drive autoimmune pathologies, such as lupus. This helps explain why two diseases categorized in distinct therapeutic areas are both potentially treatable by the same B-cell direct CAR approach.
CAR-T products with FDA approval for treatment of B cell lymphomas express receptors engineered to recognize CD19. CD19 is a marker expressed on the surface of normal B cells and a wide range of B cell malignancies. The currently approved CD-19 CAR products are autologous, ex vivo cellular therapies. These therapies are manufactured by extracting T cells from the patient’s blood, genetically modifying them in the lab, and then reinfusing them back into the same donor patient. For a significant subset of patients with B cell malignancies, CD-19 CAR- T therapies are providing excellent clinical outcomes, and in some cases elimination of the malignancy, resulting in a cure.
An expected side effect of CD-19-directed CAR-T treatment is destruction of healthy as well as malignant B cells (B cell aplasia). B cells are needed in order to mount new antibody responses against vaccines and infections, so a lack of B cells can potentially result in immune deficiency and an increased risk of infection. If circulating antibody levels become too low, they may be supplemented with immunoglobulin therapy.
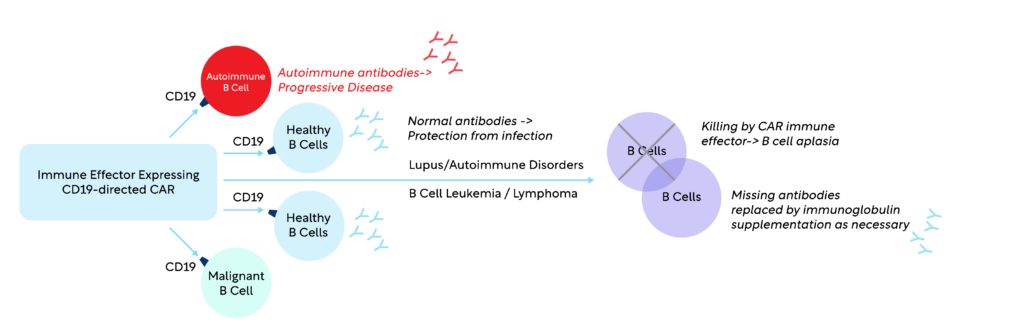
In contrast to B cell malignancies, a hallmark of lupus is not uncontrolled cellular proliferation, but rather uncontrolled production of antibodies that bind to “self” targets — in particular to nucleic acids (DNA and RNA). The level of such antinuclear antibodies often correlates with the severity of disease. Therapies that target autoreactive B cells are seen as hopeful approaches to treat lupus and similar autoimmune diseases. Investigators hypothesized that B cell aplasia produced by CD-19 CAR-T treatment, far from being a detrimental side effect, might remove B cells producing the destructive autoantibodies.
Recent publications, notably a case series published in the New England Journal of Medicine in February 2024,i cited significant clinical benefits, including alleviation of symptoms and elimination of autoantibodies. Although infections did occur, in general participants were able to stay healthy without supplemental immunoglobulin therapy. There is now increasing interest among industry and academic institutions to explore new ways to repurpose cellular therapeutic technologies from oncology indications into autoimmune disease and rheumatology.
Notably, while current FDA approved CAR products use ex vivo manufactured T cells, there is a growing interest in other CAR technology using other types of white blood cells rather than T cells—these include Natural Killer (NK) and macrophage immune effectors. Another exciting concept is moving from ex vivo (manufactured in the lab) to in vivo (generated in the body) CAR production. Some in vivo CAR-T products under development resemble mRNA vaccines in terms of drug substance, and these approaches present the potential to make CAR technology more accessible and affordable to persons with cancer and persons with autoimmune diseases like lupus.
WCG has many ways to support cell and gene therapy clinical trials for lupus. Independent Review Committees (IRBs) provide ethical oversight of all categories of clinical trials. Institutional Biosafety Committees (IBCs) oversee safe handling, storage, and administration of genetically modified products such as CAR T cells. At WCG our IRB and IBC review teams work closely together to ensure proper consideration of risks to study participants and to staff and visitors at clinical trial sites.
The Role of Scientific Review
Patient safety is an ongoing concern in all clinical trials and can be particularly challenging with the use of CAR-T therapies. When used to treat cancers such as B cell lymphomas, patients may experience adverse events such as cytokine release syndrome and immune effector cell-associated neurotoxicity syndrome in addition to secondary cancers. When using CAR-T therapies to treat autoimmune disorders, the risk-benefit assessment may be different and close monitoring of safety is critical. Data Monitoring Committees (DMCs) play a key role in guarding patient safety. DMCs review accumulating data from ongoing clinical trials to make independent recommendations to the Sponsor about the continuation, modification, or stopping of the trial. Their role is important and unique because they review cumulative and unblinded data. One of the fundamental responsibilities of a DMC is to assess the risk versus benefit of a therapy by evaluating the comparative safety in the context of efficacy. In patient populations with significant mortality, such as B-cell malignancies, a DMC may be more willing to accept an increased risk profile for a therapy when the severity of disease is high and prognosis of patients is poor. In therapeutic areas such as lupus where median expected survival is much longer than for multiple myeloma, a DMC may be less willing to tolerate an emerging safety risk for an investigational therapy.
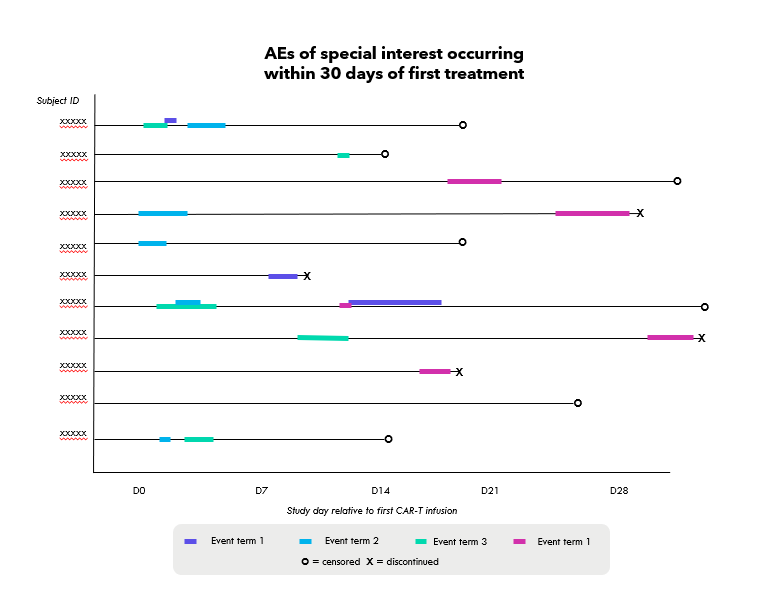
In all cases, it is crucial to ensure the DMC receives clear, accurate, and concise reporting so that the DMC can make an informed and timely decision. Design of a DMC report should reflect the data being collected, the disease under study, and the emerging pattern of risks present in the study or suspected for the class of agent. An experienced statistical reporting group recognizes the differences between interim data reporting and final analysis reports, providing the DMC with clearly written and well-structured reports that clinicians and statisticians can readily interpret. In the case of lupus trials investigating CAR-T therapies, clear and innovative techniques for summarizing and presenting data should be considered to help DMCs visualize emerging adverse event (AE) trends and ongoing safety monitoring. One example that WCG has used in reporting to DMCs is AE profile plots, plotting occurrence, duration, and severity of AEs of special interest in relationship to therapy administration and other patient disposition events. Figures such as these, see mockup below, afford the DMC the ability to review a substantial amount of data in a concise manner, where they can readily observe trends. Better detection of emerging safety signals by the DMC leads to increased vigilance in safety monitoring, and ultimately safer trials.
References
Don't trust your study to just anyone
WCG does DMCs right. Our experience, expertise, and personalized care helps sponsors organize, define, and gain insightful expertise to bridge from clinical trial to commercialization – and beyond. Experience the WCG difference starting with a free DMC services consultation.
