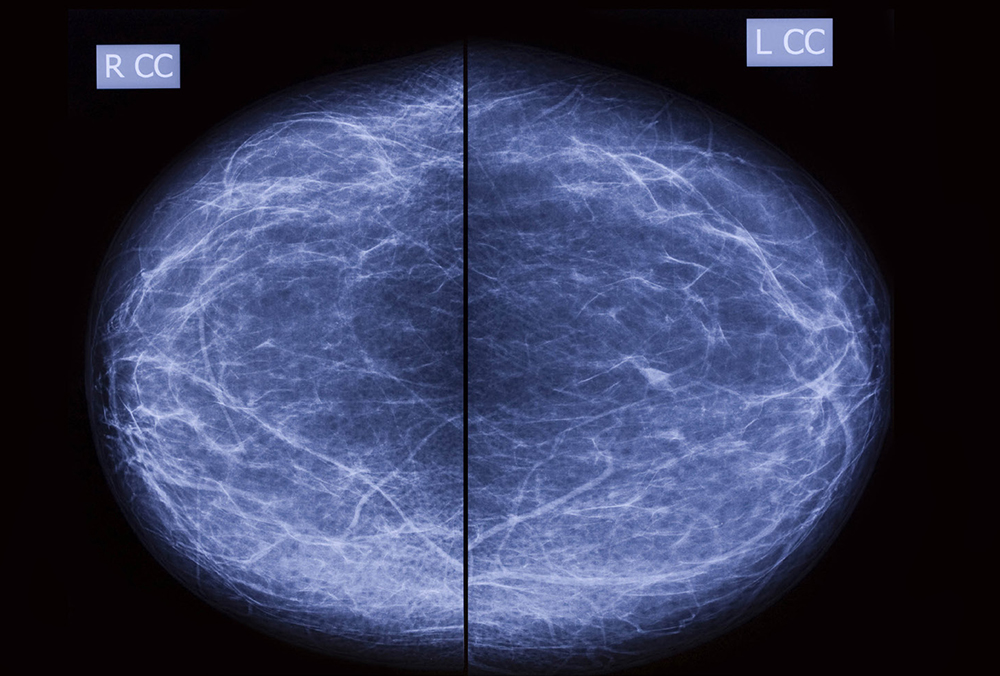
Screening mammograms have proven to be an effective means of evaluating the possibility of breast cancer in women. According to the National Cancer Institute, results from randomized clinical trials demonstrate that screening mammography can help reduce the number of deaths from breast cancer among women ages 40 to 74.
Screening Mammography CAD
Screening mammograms have proven to be an effective means of evaluating the possibility of breast cancer in women. According to the National Cancer Institute, results from randomized clinical trials demonstrate that screening mammography can help reduce the number of deaths from breast cancer among women ages 40 to 74.
The role of computer-aided detection (CAD) in screening mammography has grown in significance with the confluence of advanced software development, wide- spread utilization of digital imaging/picture archiving and communications systems (PACS), and clinical acceptance. The earliest applications of CAD in mammography were developed more than 3 decades ago, with initial pre-market approval (PMA) in the late 1990s. According to industry data, less than 40% of mammograms were interpreted using CAD in 2004 however due to increased adoption that number almost doubled by 2008. Today, it is estimated that approximately 90% of all new full-field digital mammography (FFDM) units are sold with CAD capability.
Initially, commercially available mammography CAD software products were designed for analog systems whereby mammographic images were obtained on film, digitized with a laser scanner, and analyzed using proprietary software. The computer then marked areas of abnormalities with distinct marks: one type of mark for calcifications and another mark for masses or areas of increased densities. These adjunct images were then available to radiologists for secondary assessment and either displayed on paper or on supplemental moni- tors. Since the advent of these systems, there has been a rapid conversion to FFDM (more than 80% of the US installed base has converted from analog to FFDM) and CAD marks are now most commonly displayed on soft- copy display monitors in conjunction with radiologist review.
Breast CAD systems continue to be designed and serially optimized to improve both sensitivity and specificity in the interpretation of screening mammography (studies have shown a false-negative rate of approximately 20%). The mammography CAD systems continue to be designed to assist the radiologist in assessing areas of abnormalities that may have been missed (observational oversights) and which may warrant additional assessment.
The Food and Drug Administration (FDA) PMA process requires multiple clinical studies and multiple-reader assessments. Clinical studies are typically designed to measure multiple parameters including sensitivity in the detection of microcalcifications, reproducibility, impact on work-up rates, and potential imaging benefit on the prior studies (read as normal) in patients with interval breast cancers.
Clinical Studies
The clinical results of breast CAD have not been without some controversy as the reported benefit of CAD has varied depending on the investigators. Early investigators reported an almost 20% improvement in the number of screen- detected cancers as well as an increased proportion of earlier cancer (stages 0 and 1) using CAD. Thousands of subsequent CAD publications have been written in the past decade. Some of the papers are anecdotal or technical, while some report data from several hundred thousand patients. Some indicated clear benefits of CAD. Some did not. Recently, Dr. Fenton et al published a larger retrospective review of over 600,000 patients with over 1.6M mammographic examinations and concluded that breast CAD decreases specificity but with no increase in the detection rate of breast cancer.
A review of these studies indicates that the clinical and research controversies may often be due to one or more technical limitations and that study comparisons are difficult due to variable study design. Some of the variables that have plagued investigators include: technical factors (analog vs. digital, one vs. two views, CAD algorithms), professional factors (radiologist and technologist experience), and design (retrospective vs. prospective, ‘cancer-rich’ vs. unselected patients, patient age, definition of screening mammography). One major criticism of the Fenton paper was their use of film-screen imaging techniques in a time period when this technology was being replaced by FFDM. A majority (but not all) of the publications have demonstrated increased sensitivity (reduced false negatives) but often with an increased call-back rate. Call-backs are an important aspect of clinical imaging management and call-back rates are important for several reasons: increased cost, increased radiation exposure, and increased patient anxiety. There are national guidelines for call-back rates and compliance is monitored in the clinical setting. Additionally, call-back rates are carefully monitored in the clinical trial setting and integral in FDA submissions.
Continued Market Opportunity
Controversies aside, the use of CAD in screening mammography does hold great promise. The sensitivity in the detection of calcifications is the major contribution of CAD (over 90% sensitive in most studies).The detection of abnormal masses or densities is also high (75-85%). Detection of areas of architectural distortion could use improvement and currently ranges between 35-50%. Overall (depending upon study and design) the detection rate is 80-90%.
Using CAD software available today, there is, on average, more than one CAD mark on each of 4 images obtained during a routine bilateral screening mammogram. Though the improvements in both CAD processing and mammographic imaging have steadily improved, a vast majority of the CAD marks reported will still be determined to be benign. One study estimated that as many as 2,000 marks will need to be assessed and cleared by a radiologist to detect a single “true-marking” of a breast cancer. There are trade-offs both in clinical trials and in a clinical setting between sensitivity and specificity for both mammography (and other breast imaging) as well as for CAD. The receiver operating characteristic (ROC) curve is carefully studied in clinical trials to assess the potential benefit of CAD. Some commercial CAD products permit some end-user (radiologist) adjustment in these measures.
Errors in radiographic interpretation can be grouped loosely into 3 categories: perception, analysis, and technical. Each can be influenced by many variables. The CAD clinical trials have largely emphasized greater detection (perception) as end-points while placing the burden of analysis (or significance) on the radiologist. While technical issues may result in both false positive and false negative CAD assessments, this variable has not been studied to any significant degree in clinical trials.
In attempts to improve the detection of mammographically- visible breast cancer, some radiologists migrated to double- reading mammograms (two independent readers) with reported improvement in detection of 5-15%; improvements that may now be achievable with a single radiologist using CAD. The recall rate of patients for additional imaging has been shown to increase with both reading protocols, though increases in sensitivity and cancer detection have also been shown. Many practitioners self-report an initial increase in call-back rates following implementation of CAD, which gradually decreases over time. Clinical trial protocols, particularly those containing a conversion in the utilization of CAD, may not fully capture these trends.
Summary
Over the last 10 years, screening mammography has been shown to be the most effective tool in screening for breast cancer and has been shown to decrease the mor- tality of breast cancer by over 30% and is the most wide- spread tool in preventing breast cancer deaths. A market opportunity exists for developers with improved screening mammography CAD algorithms to further assist the radiologist in diagnosing breast abnormalities. This coupled with further advances in FFDM, radiologist expertise, and eventual application to 3D mammography (tomosynthesis), should continue to improve the early detection and sub- sequently, the successful treatment of breast cancer.
Volume 4, Issue 2: Guidance For Sponsors: Screening Mammography CAD: A Continued Market Opportunity
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.