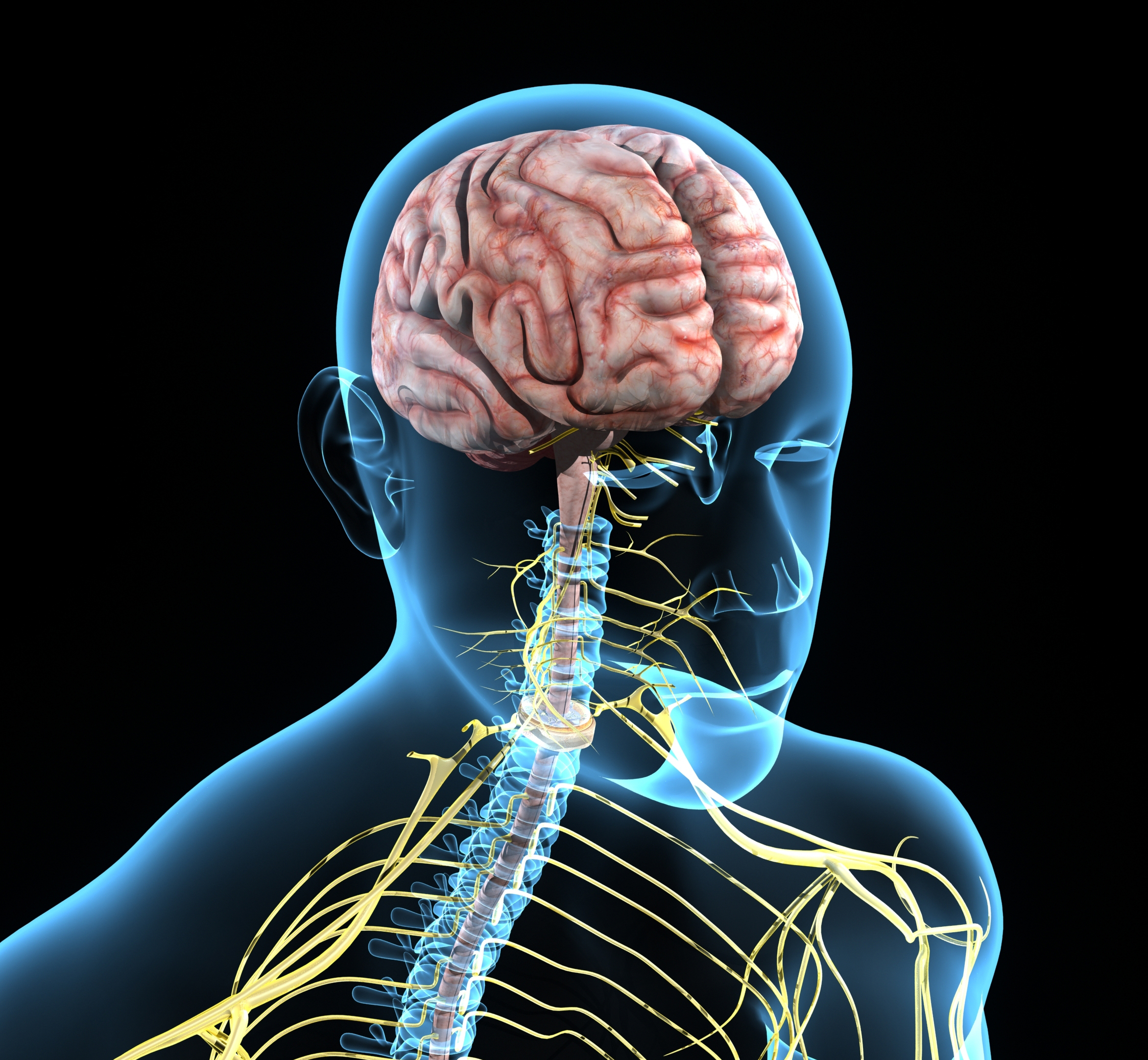
There have been several revolutionary advancements in the field of neurological imaging. These have included the invention of Computed Tomography (CT) and Magnetic Resonance Imaging (MRI), as well as the introduction of intravenous contrast enhancement. These techniques are the foundation of noninvasive neurological imaging and have advanced patient clinical care and research.
Magnetic Resonance Imaging in particular provides exquisite differentiation of various tissue types and fluids. MRI has the advantage of using magnetic fields and radio frequency energy rather than ionizing radiation. This eliminates the risk of inducing DNA defects leading to cancer that is inherent to X-rays and CT imaging.
Contrast Agents
Along with the development of MRI imaging protocols,
contrast agents were also created to enhance the identification of intracranial pathology. Contrast enhancement enables exceptional visualization and delineation of tumors and other pathology of the brain. When designing clinical trials, one must ensure the multitude of enhancement patterns are considered in order to create a robust and meaningful study. Following the response of enhancing lesions has been an invaluable tool in clinical studies to determine the effectiveness of medical therapy. This allows for a noninvasive and rapid assessment of therapy. Development of new lifesaving therapies are accelerated by having quicker measurement of clinical trial endpoints. Clinical treatments may be also be quickly modified if a patient is no longer responding to the current therapy.
Most contrast agents use the paramagnetic ion, gadolinium. Gadolinium based contrast agents (GBCA) work by altering the tissue response to radio frequency pulse energy absorption and emission while in the magnetic field of the MRI scanner. The contrast agent shortens the time it takes for the surrounding protons to relax back to the orientation of the MRI magnetic field once the radio frequency pulse is switched off. This shortening is imaged as increased signal on T1-weighted imaging and highlights tumors and other enhancing pathology of the brain.
Gadolinium ions are chelated, or attached to larger organic molecules forming stable nontoxic complexes. GBCAs circulate through the vascular system and pass rapidly into the interstitial compartment and are then cleared from the body mainly by renal excretion.
GBCAs can be categorized based on the geometry of its chelating agent: Linear or Macrocyclic. Macrocyclic chelating agents are much more stable than the linear class and therefore, have less dissociation of gadolinium ions. The dissociated free gadolinium ions are toxic and have been associated with the development of a rare, but serious disease called nephrogenic systemic fibrosis (NSF). Excess linear chelating agents are added to the formulation to help bind free dissociated gadolinium ions. Macrocyclic agents bind their gadolinium ions so tightly no excess agent is needed. Chelating agents can be further subdivided as ionic or non-ionic. In general, ionic chelates are more stable than non-ionic chelates.
Enhancement of brain lesions occurs through two routes; intravascular and interstitial. Intravascular enhancement is due to vasodilatation or neovascularity and is related to increased blood flow or blood volume. Interstitial enhancement occurs due to a breakdown in the blood-brain barrier. GBCAs injected into the blood stream do not cross the intact endothelial blood-brain barrier. GBCAs will concentrate in tissues with a disrupted endothelial barrier, such as tumors, infection, and inflammation. Contrast will also accumulate in tissues without a blood-brain barrier, such as the meninges.
When designing protocols for clinical trials, there are important considerations when using contrast enhanced MRI. MRI enhancement follows a distinct set of patterns that are invaluable in characterizing lesions of the brain. By understanding and accounting for these patterns, appropriate evaluation and categorization of lesions will enable the success of the trial.
Extraaxial Enhancement
Enhancement should be first defined as intra- or extraaxial. Extraaxial enhancement may be smooth or nodular. Thin smooth extraaxial pachymeningeal enhancement is seen with dural vasodilatation associated with intracranial hypotension and postoperative change. Focal or nodular pachymeningeal enhancement may indicate neoplasm, such as meningioma, metastatic disease and lymphoma. Granulomatous disease also displays nodular enhancement.
Extraaxial leptomeningeal enhancement on the surface of the brain and in the sulci is often due to infection from bacterial, viral, or fungal meningitis. Neoplastic leptomeningeal enhancement, termed carcinomatous meningitis, is a dreaded form of metastatic disease often from breast cancer or lymphoma, as well as primary CNS tumors.
Intraaxial Enhancement
Intraaxial enhancement is subdivided based on its location. Starting outward and working centrally, the first pattern is gyral enhancement. Serpentine gyral enhancement of the gray matter often has a vascular or inflammatory etiology. Vasodilatation may follow seizures, ischemia or infarct reper- fusion, and posterior reversible encephalopathy syndrome. Inflammatory processes of meningitis or encephalitis show enhancement related to a disrupted blood-brain barrier.
Subcortical nodular enhancement often represents hematogenous spread of metastatic disease or septic emboli. The lesions may be solid or ring enhancing and are often small at time of discovery because they involve the gray matter of the adjacent cortex.
Deep ring enhancing lesions involve the white matter and deep gray structures. Deep ring enhancing lesions have the following etiology; glioma > metastases > abscess > demyelination. High grade tumors of gliomas and metastases have a thick irregular ring of enhancement related to central necrosis. Abscesses produce a thin smooth complete ring of enhancement. Active demyelination enhancement is often an incomplete ring and may be faint and have ill defined margins.
Enhancing nodule with associated cyst pattern is produced by low-grade fluid secreting tumors. This pattern may be quite heterogenous and is often associated with pilocytic astrocytomas and hemangioblastomas in the posterior fossa. The solid nodule enhances and the rim of the fluid “cyst” usually does not. Tumors with this pattern in the supratentorial brain include pilocytic astrocytoma, pleomorphic xanthoastrocytoma, ganglioglioma, and ependymoma. Periventricular enhancement with a thick solid pattern is seen with primary CNS lymphoma and primary glioma. These two neoplasms often cross the corpus callosum. Thin smooth periventricular enhancement is associated with infections of ependymitis and ventriculitis.
Summary
In summary, modern non-invasive neurologic imaging has been made possible with the advent of CT and MRI scanning. Intravenous contrast agents are an indispensable tool used in the categorization of central nervous system lesions. Gadolinium based MRI contrast agents provide critical diagnostic information to help guide the clinical care and therapy of patients on a daily basis. Clinical trial de- sign must account for the various enhancement patterns of brain lesions to create consistent and reliable data. Mean- ingful scoring criteria and measurement protocols can be tailored to the type of lesion enhancement encountered in the trial. Successful trial design depends on a thorough understanding of the physiology and patterns of contrast enhancement.
Volume 6, Issue 7: Guidance for Sponsors: Neurological Imaging: Contrast Enhancement in Clinical Trials
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.