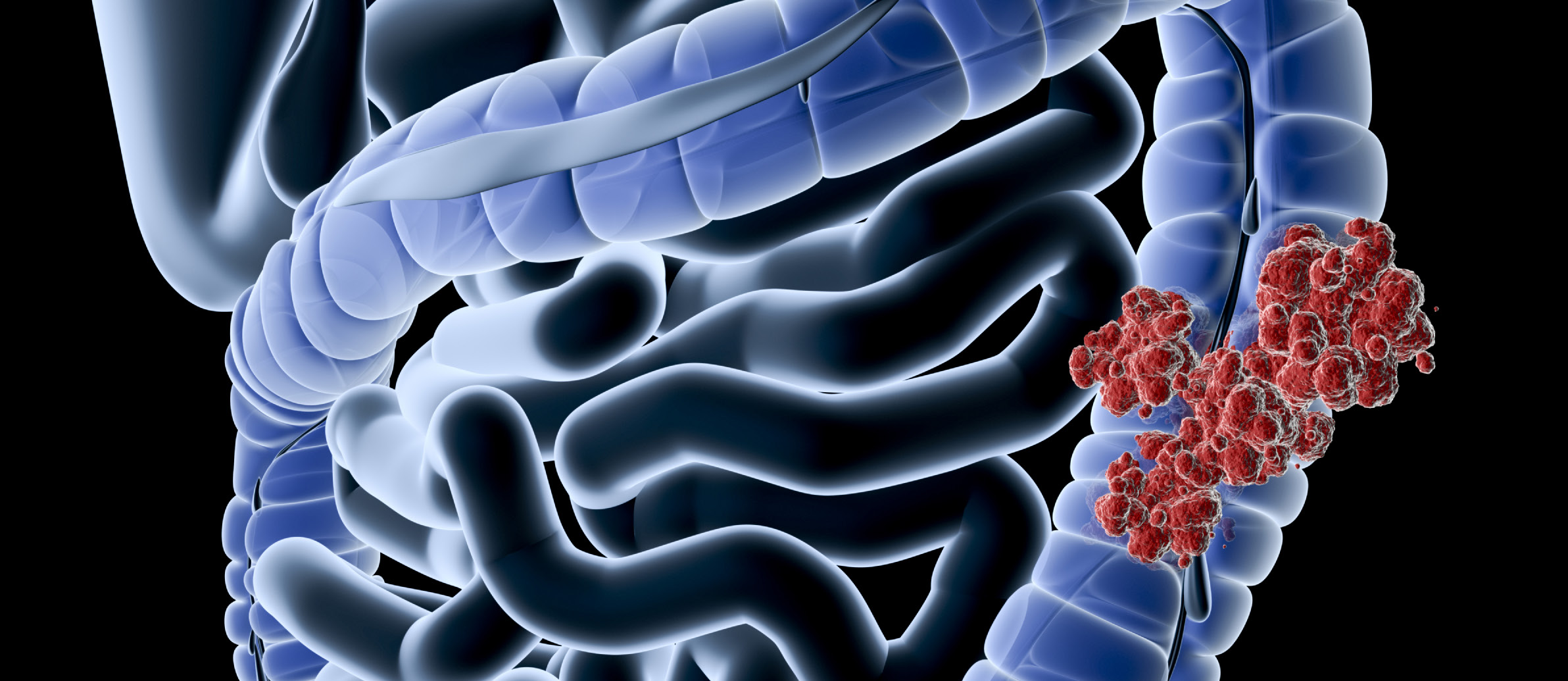
Colorectal cancer (CRC) is the second leading cause of cancer- related deaths in cancers affecting both men and women in the United States. In 2007, the most recent year for which statistics are compiled, 142,672 new cases of CRC were diagnosed in the United States concurrently with 53,219 deaths. It is estimated 1 in 6 of patients diagnosed with CRC will have metastatic disease at presentation and 50% will develop metastatic disease (mCRC) during the course of their treatment.
An evaluation of the evolution of therapy over the last twenty years demonstrates significant improvements in prognosis with patients diagnosed with mCRC. In the past, patients, meeting rigorous inclusion criteria with metastatic liver disease, could undergo surgical resection and achieve a potential route to cure with a 5-year survival of 30-40%. Unfortunately, this complement of patients with easily resectable disease limited to the liver accounted for only 10% of mCRC patients. The remainder of patients at the time had very low 5-year survival rates as chemotherapy
alone was the only potential offering to these patients.
Conventional Treatment Regimens
The progression of medical research and clinical trials has brought the advent of several new compounds focused towards treatment of this disease process. Oxaloplatin, irinotecan (FOLFOX/FOLFIRI) and new targeted agents (bevacizumab, cetuximab and panitumumab) have increased response rates of mCRC up to 60%. The utilization of pre- operative chemotherapy has allowed previously designated unresectable patients to undergo resection, although with less favorable outcome postoperatively as compared to patients with limited disease. The goal of many new therapies has now evolved to allow a bridge to liver resection as this remains the best chance for cure. Sadly, improved clinical response with better treatments has not necessarily correlated with improved outcome. The struggle continues to achieve long-term survival in those patients with metastatic disease. Despite the progress of drug development and clinical research, the complement of these new agents coupled with aggressive surgical intervention still relegates mCRC patients to a low 2-year survival rate of approximately 40%.
Complete Pathologic Response
In current therapy, clinical response is measured by radio- graphic analysis with complete clinical response standing as a surrogate for complete pathologic response (cPR). Complete clinical response will correlate with increased median survival but has a limited ability to predict disease cure. Neither complete disappearance of a lesion by CT nor complete loss of metabolic activity on PET reliably predicting complete pathologic response. On the contrary, complete tumor eradication and clinical cure has been observed in some cases regardless of whether the initial tumor site resolves on follow-up radiographic imaging. The achievement of complete pathologic response, although rare, has been shown to better correlate with improved long-term clinical survival.
In one series, complete pathologic response was found to occur in only 4% of patients resected for liver only mCRC after receiving preoperative chemotherapy. However, those patients who were able to achieve this goal had exceptionally long-term survival. There were multiple factors predicting complete pathologic response, but primarily this goal was achieved in those patients presenting with small tumors (less than 3 cm), relatively low CEA levels (less than 30 ng/ mL) and patients younger than 60 years of age. Overall, the presence of these three predictive factors was associated with an increased proportion of patients achieving complete pathologic response (approximately 1 in 3) and 5 year survivals of an incredible 76%.
The goal among practitioners treating mCRC patients is complete pathological response. However, achieving this goal with chemotherapy as a sole treatment agent is fraught with complexity given the multifactorial nature of the disease. First, complete pathological response cannot be measured based solely on clinical response as the two are not necessarily equal; pursuing this goal may increase the risk of tumor progression, after an initial response, if it delays curative liver resection. Second, the duration of chemo- therapy before surgery has an inversely negative impact on outcome in patients after surgery. The longer chemotherapy is administered trying to achieve a complete clinical response, the higher the risk of postoperative complications related to hepatotoxicity which results in lower survival rates after resection. Thus the prolonged administration of additional chemotherapy does not necessarily improve responses or outcomes.
The addition of Vascular Endothelial Growth Factors (VEGF) inhibitors such as bevacizumab has been shown to improve clinical responses to chemotherapy. For patients who fail these initial regimens, the additional use of Endothelial Growth Factor (EGF) receptor inhibitors can be helpful. While helpful for those treating mCRC, this strategy has its limitations as a combination of both VEGF and EGF inhibitors creates a regimen that is actually detrimental to patient outcomes. These challenges serve not only as a motivator to continue to develop better biologics, but have spurred the development of other novel treatment strategies.
Locoregional Therapies
Although the evolution of systemic medical therapies has improved outcomes, researchers continue to develop adjunctive therapies given the inability to achieve cure with these biologics alone. The logical next step has been the addition of local regional therapy to systemic chemotherapy. A targeted therapy limited to the liver should increase the response rate within the liver and therefore improve the odds of achieving complete pathologic response and avoid some of the downside of prolonged chemotherapy administration.
The practice of locoregional therapies encompasses the delivery of chemotherapy or radiation to disease within the liver. The two main treatment strategies are Transarterial Chemoembolization (TACE) and Complex interstitial brachytherapy with yttrium-90 microspheres.
Currently, the SIR-Spheres yttrium-90 product is an FDA approved treatment for unresectable metastatic liver disease from primary colorectal cancer with the adjuvant use of intra-hepatic arterial chemotherapy of Floxuridine. Users of this combined therapy have shown improved response documented by radiological follow-up and increased median survival of treated patients. This therapy, however, has not been supported by a randomized controlled trial demonstrating survival benefit for mCRC patients receiving systemic chemotherapy. Despite receiving FDA approval 10 years ago, it has not established a major role in treating mCRC due to this lack of proven benefit and because of limiting utilization factors such as cost and the need for specialized centers for delivery.
Trans-arterial chemoembolization of the liver without systemic chemotherapy has been shown prospectively to prolong survival and retrospectively to increase complete pathologic response in hepatocellular carcinoma (HCC). In colorectal carcinoma, TACE has been an effective third line therapy for mCRC patients failing chemotherapy, although in single arm studies.
Logically, simply combining TACE with systemic chemo- therapy in an additive manner should increase the prevalence of a complete pathologic response. Synergistically there are other reasons to expect this outcome, particularly, if VEGF inhibitors are included in the regimen. The utilization of locoregional therapy with chemoembolization has been shown to increase the expression of VEGF receptors on tumor cell membranes in HCC and Hypoxia Induced Factor 1a in VX2 mouse tumor models. This finding implies that the addition of bevacizumab or other VEGF receptor targeting agents should improve the effectiveness of therapy beyond the sum of their parts. Translating this hypothesis, of an increased rate of complete pathologic response that ultimately improves long-term outcome, into practice will require randomized controlled clinical trials that, not only measure tumor response rates but, also document complete pathologic response and 5-year survival.
Hepatocellular Carcinoma As A Basis
A review of the work done with HCC demonstrates a paradigm that can be applied to the treatment of mCRC. First, two randomized trials established that conventional TACE would improve survival. Second, the Precision-V trial showed chemoembolization with doxorubicin drug-eluting beads was superior to conventional ethiodol based chemoembolization. The results of this trial have now established Precision-TACE as the standard of care for HCC amongst those who deliver this sub-specialized care.
Extrapolating from this data, interventional radiologists have been using drug eluting beads loaded with irinotecan (DEBIRI) instead of doxorubicin for the treatment of mCRC. The utilization of drug eluting beads can both simplify and unify the TACE technique across multiple institutions particularly when standard doses are specified for delivery during each session.
Preliminary Trial Data And The Need For Further Work Preliminary trials to date suggest that DEBIRI can increase the complete pathologic response in patients which should contribute to increased long-term survival. Combined with hepatic resection of metastatic disease, DEBIRI should then also increase the chance for a curative procedure. As such, patients under consideration for surgical intervention would likely benefit from treatment, not because their unresectable status could be downstaged to surgical status, but because DEBIRI in addition to systemic therapy could provide a higher rate of complete pathologic response and therefore higher rates of ‘curative’ 5 and 10-year survivals. Unfortunately, this protocol of DEBIRI as first-line therapy in combination with chemotherapy for patients with metastatic disease undergoing hepatic resection has not been prospectively evaluated. Unlike HCC, no survival benefit has been demonstrated to support making it the standard of care.
DEBIRI therapy has also been used anecdotally as salvage therapy for patients failing chemotherapy. Here again, no randomized prospective trials have been performed investigating its possible utility in treating patients with mCRC receiving 3rd-line therapy. Patients expressing mutant KRAS genes in their tumors may show particular benefit in 3rd-line therapy trials as these patients are less likely to respond to EGF inhibitors like cetuximab or panitumumab.
We believe these two groups of patients offer the best opportunity for 1st and 3rd line therapy investigations and should be the priority for future randomized clinical trials evaluating DEBIRI therapy in mCRC.
Questions Regarding Techniques In Trials
The Precision-V trial demonstrated that the operator’s technique is important for success and that delivery mechanisms could be simplified. Previous TACE trials included such an array of variable techniques to perform the same procedure that it wasn’t alway clear how to explain the differing results found. This lack of standardization has limited our ability to make helpful observations to guide clinical practice. Many questions remain to be explored in terms of the techniques utilized for locoregional therapies. Is there an optimal particle size to use? Do smaller particle sizes that penetrate deeper into tumors afford an advantage to the patient? How selective should radiologists be when targeting tumors? Do fifth and sixth order embolizations, which are more difficult and time consuming, result in better outcomes as they spare non- target normal liver tissue and concentrate treatment in the tumor? How important is tumor vascularity in determining success? It is believed that vascular tumors respond more readily to embolization, but is this important in predicting complete pathologic response or long-term survival?
Many TACE trials do not address these details, yet these technical components are important in helping medical scientists understand the mechanisms as well as outcomes. By studying more of these factors, radiologists can help increase the homogeneity in application of this highly operator dependent technique across institutions and patients.
Summary
Although locoregional therapies like DEBIRI should have established roles in the treatment of mCRC, they don’t because they are not supported by randomized prospective clinical trial data. Current proponents and practitioners using these therapies lack trial data to demonstrate true superiority in both patients under consideration for surgical intervention as well as mCRC patients receiving 3rd- line therapy. There remains work to be done in this area to benefit patients suffering from this widespread disease.
Volume 6, Issue 8: Guidance for Sponsors: Metastatic Colorectal Cancer and Locoregional Therapies
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.