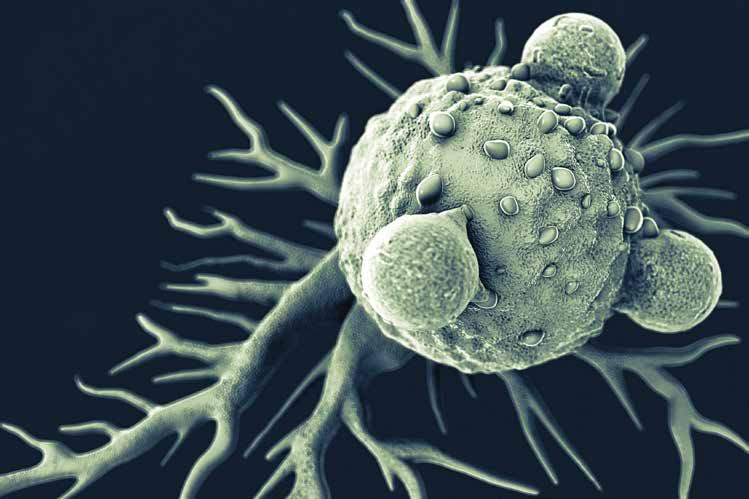
Over the past several decades of immuno-oncology research, there has been evidence that tumor cells can be recognized by the native immune system. Immune modulation in cancer refers to a range of treatments aimed at harnessing the patient’s immune system to achieve tumor control, stabilization, and potential eradication of disease.
Immuno-Oncology
Over the past several decades of immuno-oncology research, there has been evidence that tumor cells can be recognized by the native immune system. Immune modulation in cancer refers to a range of treatments aimed at harnessing the patient’s immune system to achieve tumor control, stabilization, and potential eradication of disease. This has led to the development of therapies that permit specific tumor destruction without toxicity to normal tissue. It also has the potential to prevent tumor recurrence as a result of the immune systems long-term memory.
Recently, immuno-oncology therapies have been found to provide lasting anti-cancer benefits to patients who have previously had very few treatment options available to them. These therapies thereby have the potential to revolutionize and become an important part of future oncology treatments.
The main categories of immuno-oncology therapies being developed include monoclonal antibodies, cancer vaccines and non-specific immunotherapies. Several immuno-oncology therapies are in the process of being approved by the Food and Drug Administration (FDA) and others are being evaluated in clinical trials. These immune based therapies hold great promise for the treatment of malignant melanoma, lung, colorectal, renal and prostate cancer as well as many others tumor types.
A vital component of any cancer treatment is the objective assessment and monitoring of tumor response to anticancer therapy using imaging and specific response evaluation criteria. As immuno-oncology therapies continue to be developed and undergo testing in clinical trials, consideration needs to be given to the differences observed in tumor response following immunotherapy.
RECIST
With the exception of malignant lymphoma, the Response Evaluation Criteria in Solid Tumors (RECIST) guidelines published in 2000 and revised in 2009 have become the most widely accepted criteria for most solid tumor response assessments in clinical practice and in clinical trials.
In general, RECIST provides a standardized and practical method to assess response and progression in solid tumors. However, as the criteria was developed to evaluate response to treatment with cytotoxic chemotherapeutic agents, there are some limitations in its application and response assess- ment in novel cancer treatments. For example, a limitation when using RECIST is that an early increase in tumor size, or the appearance of new lesions, is classified as progressive disease and classifies as a treatment failure. In studies, however, with immunotherapeutic agents (e.g. Ipilimumab), clinical experience has shown that complete response, partial response, or stable disease status can still be achieved after an initial increase in overall tumor burden. Thus, RECIST may not be sufficient to fully characterize tumor response and progression in patients treated with specific targeted oncology therapies or in tumors that are being targeted by different anticancer pathways.
To overcome the limitations of RECIST, several other response criteria have been developed for specific types of cancer treated with specific immunotherapeutic agents.
irRC
Ipilimumab, a fully human monoclonal antibody (IgG1) exerts the anti-tumor activity by augmenting the body’s immune response to cancer cells. This is achieved by the activation and proliferation of T cells, which, rather than direct cytotoxic effects, leads to tumor infiltration by T cells and ultimately tumor regression. T lymphocyte antigen–4 (CTLA4) is an immune checkpoint molecule that down-regulates T-cell activation. Ipilimumab blocks CTLA4 and thereby augments the T-cell immune response to cancer cells.
Clinical observations of advanced melanoma patients treated with ipilimumab suggested that conventional response assessment criteria such as RECIST criteria were not sufficient to fully characterize patterns of tumor response to immuno- therapy, because tumors treated with immunotherapeutic agents may demonstrate additional response patterns that are not described by these conventional criteria.
While conventional responses are seen with immunotherapy, often response to immunotherapy is noted to occur after an initial increase in tumor burden. Further, regression of initial lesions may occur despite development of new lesions. Using the RECIST criteria, the patient would have been classified as having progressive disease when in fact there has been a positive response to the immunotherapy.
Developed in 2009, the Immune-related Response Criteria (irRC) was developed based on an understanding of the regulatory pathways of the immune systems response to cancer. As such, the irRC is well suited to evaluate metastatic melanoma patients treated with immunotherapeutic agents such as ipilimumab. The irRC was intended to specifically define the response patterns that are observed in patients receiving immunotherapy and to identify successful treat- ment outcomes that would be missed by the RECIST criteria.
The initial apparent increase in tumor burden preceding response can be due to either tumor growth until a sufficient immune response develops, or transient immune cell infiltrate with or without edema. In addition, apparent new lesions may be due to T cell infiltration into radiographically undetectable tumor deposits that are already present at baseline. irRC criteria enabled capturing patients who show response patterns that are not detected in the conventional criteria but still benefit from therapy.
The novelty of irRC is that it considered the patient’s ‘total tumor burden’ and required confirmation of suspected disease progression with subsequent imaging, approximately four weeks later. irRC has been used in tandem with conven- tional response criteria such as RECIST and in current clinical protocols for prospective validation of immunotherapeutic agents such as ipilimumab. Although the development of the irRC was based on patients with advanced melanoma treated with ipilimumab, more recent studies have proposed the application of irRC in other types of cancer, including renal cell carcinoma, non–small-cell lung cancer, and prostate cancer treated with novel immunotherapeutic agents.
RECIST versus irRC
While RECIST uses unidimensional measurements, the irRC utilizes bidimensional tumor measurements of target lesions, which is obtained by multiplying the longest diameter and the longest perpendicular diameter of each lesion at baseline assessment.
At each subsequent follow-up assessment, the sum of the products of the two largest perpendicular diameters of the target lesions as well as that for new measurable lesions (≥ 5 × 5 mm) are included to reflect the total tumor burden. This is in distinct contrast to the RECIST criteria, which does not measure new lesions and results in progression with the occurrence of a new lesion. With RECIST, patients with an increase in tumor burden by either ≥ 20% of measured target lesions unidimensional measurements or with an unequivo- cal new lesion, are considered as progressed and as such a treatment failure, irrespective of time interval considerations since first treatment. With irRC, patients are not assessed as having progression even if new lesions are present, as long as the tumor burden of all lesions does not increase by 25% or more. In addition, patients are considered to have partial response or stable disease even if new lesions are present, if they meet the thresholds of response. In the absence of rapid clinical deterioration, the irRC criteria also requires confirmation of progressive disease by a second scan within 4 weeks after initial progressive disease to capture late-responding patients with a trend toward treatment response.
irRECIST
While RECIST measures fewer numbers of lesions unidimensionally (5 target lesions in RECIST 1.1) versus irRC which measures a greater number of lesions bidimensionally (10 target lesions), irRC has the advantages of not progressing the disease prematurely when the treatment effect may not be fully evident. In addition, studies have demonstrated that irRC unidimensional measurements, when compared to bidimensional measurements, are more reproducible, have less measurement variability and result in lower misclassification rates for response assessment. In order to utilize both the established criteria advantageously, the two systems have been adapted and modified with the combination of
RECIST and irRC into irRECIST.
Immune-related Response Evaluation Criteria In Solid Tumors (irRECIST) is a recently established and published measurement guideline that is expected to provide better assessment and more reliable and reproducible study data for targeted immunotherapeutic agents in oncology studies. The adapted irRECIST criteria are modifications to the irRC, incorporating the advantages of RECIST and at the same time overcoming shortcomings of the standard RECIST criteria. irRECIST adaptations include, but are not limited to, unidimensional measurements, inclusion and assessment of all detected lesions and avoiding early declaration of progressive disease.
irRECIST is an innovative step which is expected to be simpler, more reproducible and less ambiguous to assess efficacy and effectiveness of immunotherapeutic agents, and provide response assessment that can be directly compared with the results from clinical trials in the past decade.
Conclusion
It has long been recognized that the immune system plays an important role in the suppression of cancer. Utilizing the immune system to eliminate cancer holds great potential. Ongoing research has demonstrated that immunotherapeutic agents can significantly improve survival and clinical outcomes in patients with several types of cancer. Modified imaging criteria have been developed to capture these novel clinical responses associated with immune therapies.
With advanced understanding of the application and results of established assessment criteria, adaptation in the form of irRECIST is a step to further optimize the approach to evaluate response to treatment in patients receiving cancer immunotherapy.
Volume 5, Issue 5: Guidance For Sponsors: irRECIST and Immuno-Oncology in Clinical Trials
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.