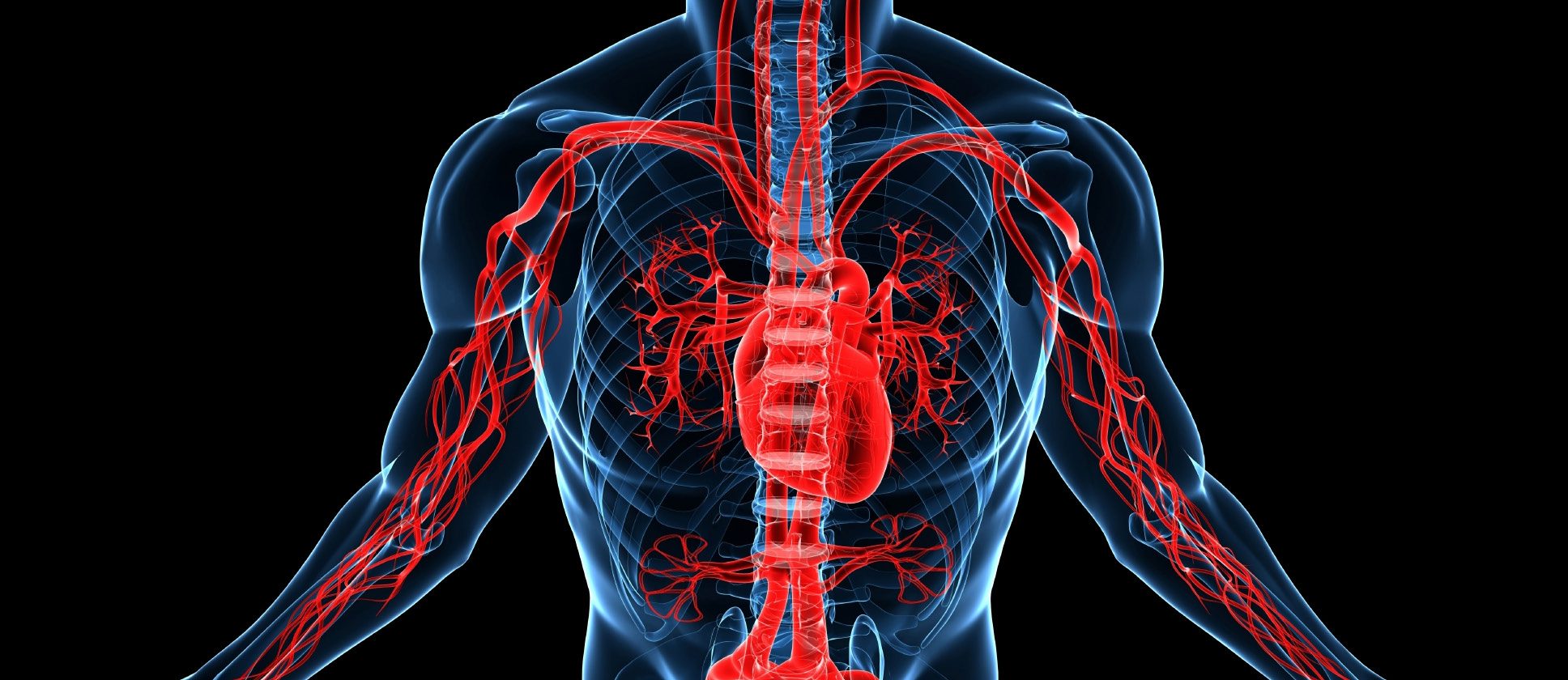
Venous thromboembolic disease begins in areas of blood stasis, typically in valve pockets in the deep veins of the lower extremities. Under favorable conditions, the clot propagates centrally to reach the iliac veins and inferior vena cava. Pulmonary emboli occur when a portion of the thrombus breaks off and passes through the heart into the pulmonary arteries. The emboli obstruct blood flow to the lungs and deprive the patient of oxygen. Death is often sudden, frequently without warning. Chronic or repetitive emboli lead to pulmonary hypertension, a severely disabling disorder.
Venous Thromboembolic Disease
Venous thromboembolic disease is a serious condition afflicting over one million patients per year in the United States where it is the third most common cardiovascular disorder. Pulmonary emboli are the end result of this entity and they kill up to 200,000 patients per year.
Venous thromboembolic disease begins in areas of blood stasis, typically in valve pockets in the deep veins of the lower extremities. Under favorable conditions, the clot propagates centrally to reach the iliac veins and inferior vena cava. Pulmonary emboli occur when a portion of the thrombus breaks off and passes through the heart into the pulmonary arteries. The emboli obstruct blood flow to the lungs and deprive the patient of oxygen. Death is often sudden, frequently without warning. Chronic or repetitive emboli lead to pulmonary hypertension, a severely disabling disorder.
Pulmonary emboli are often associated with hospitalization. Risk factors include recent surgery, malignancy, trauma, limited mobility associated with neurological disorders, obesity, atherosclerosis, and hypercoaguable states that can be hereditary or related to hormonal therapy. Pregnancy is a risk factor. The incidence of this disorder rises with age and is prevalent in the elderly. Pulmonary emboli are often recurrent.
Thromboembolic disease is often difficult to diagnose clinically and may have few symptoms prior to a fatal embolism. D-dimer assays are a blood test used to screen for clot degradation products in the patient’s blood. However, this test lacks sensitivity and has poor specificity. Venous ultrasound exams of the lower extremities are used to search for blood clots in the veins and CT angiography is the principal imaging study to identify pulmonary emboli in the lungs. These imaging studies are sensitive and highly specific. They can be used both for diagnosis and to track the progress of therapy by measuring the clot burden and distribution.
Anticoagulation has long been the mainstay of therapy for thromboembolic disease. By stabilizing the propagation of the thrombus, anticoagulants reduce the risk of pulmonary emboli. Unfortunately, anticoagulants have the potential for serious bleeding complications and have many contraindications. This led to the concept of mechanical filtration of blood flow to protect the patient from pulmonary emboli.
Inferior Vena Cava Filtration
The initial attempts at mechanical filtration began about 1930 and involved surgical ligation of the iliac veins and inferior vena cava. This strategy proved ineffective with high morbidity and many complications. The need for a more effective therapy led to the development of the Greenfield Inferior Vena Cava filter in 1973. This metal filter was designed to provide permanent IVC filtration and was initially placed by an open surgical approach. It was shown to be highly effective in protecting patients from pulmonary emboli. A percutaneous delivery system for this device was introduced in 1984, thus inaugurating the modern era in mechanical filtration for the treatment of pulmonary emboli.
It soon became apparent that not all patients needed permanent IVC filtration. Many of the clinical indications for placement were temporary. It was also clear that much further development was needed to refine the design of these lifesaving devices. Early research identified that an ideal filter should be effective at trapping even small emboli so as to avoid the development of pulmonary hypertension. It should also be biocompatible and nonthrombogenic while maintaining structural rigidity and durability. An ideal filter should be easy to deliver into proper position and stay where it is placed. At the same time, it must not damage the inferior vena cava and should have the option to be retrieved, so that it can be removed when the risk of embolization has passed.
Introduction of new filter designs in the United States is subject to 501k premarket approval by the Food & Drug Administration. Pre-clinical testing is required to document biocompatibility and filter performance of the new device. Clinical trials must be performed to establish the efficacy of the new device as compared with existing filters currently on the market. Careful consideration must be given to use an appropriate hypothesis and study design with sufficient sample size to arrive at a meaningful conclusion. It is essential that the range and rate of complications related to the new device be established and thoroughly analyzed.
In addition to the physical development of the device, much work continues to be done to refine the indications for mechanical filtration. Initially, filters were placed permanently into patients with thromboembolic disease and a significant contraindication to anticoagulation. As filter design has improved to make placement and retrieval safer, the indications for the use of these filters has continued to evolve and expand. The prophylactic use of retrievable filters in patients at high risk for development of thromboembolic disease is an active area of current research. The Society of Interventional Radiology issued a special communication from a multidisciplinary research consensus panel in 2009 identifying their highest priority was to initiate a multicenter randomized trial to establish the efficacy of the prophylactic use of retrievable filters in trauma patients.
Radiologists are integral to the diagnosis and management of thromboembolic disease. Venous ultrasound of the lower extremities has become the mainstay of imaging to diagnose the presence of deep venous thrombi that progress to pulmonary emboli. Modern multidetector CT scanners produce pulmonary angiograms in a single breath hold with sufficient resolution to identify even small peripheral emboli. These scanners are also capable of assessing the extent of thrombus propagation into the iliac veins and the inferior vena cava. Once the diagnosis has been made, Interventional Radiologists utilize digital Special Procedure Suites to precisely place and document the deployment of the indicated filter and will then retrieve that filter when indicated.
Summary
There remains much research to be performed to perfect the design, and to refine the indications for use, of these devices to provide mechanical filtration for the treatment of venous thromboembolic disease. Radiologists play a critical role in this research process as well as being integral to the management of this disorder. They have the experience and expertise to guide clinical trials to select the best imaging protocols to evaluate the next generation of retrievable IVC filters. Advanced imaging will be essential to establish the precise localization of filter deployment, the amount of thrombus capture by the device and the presence on any pulmonary emboli that escaped entrapment by the filter. Successful clinical trials will require close collaboration between Diagnostic Radiologists and Interventional Radiologists who possess a broad experience in the diagnosis and management of thromboembolic disease.
Volume 6, Issue 10: Guidance for Sponsors: Inferior Vena Cava Filters: Medical Imaging in Clinical Trials
Originally written by legacy Intrinsic Imaging Medical Director
Contact WCG Imaging to discuss your trial’s imaging needs
We have the team, therapeutic expertise, technology, and ISO-certified quality management systems to provide imaging core lab services to our clients worldwide. Complete the form to get started.